An Overview of Risk and Prevention

In addition to cardiac events, another life-threatening side effect has been associated with the Pfizer-BioNTech vaccine. When is the risk period? Does the flu shot play any role in these events? What actions should we take to better protect ourselves?
Summary of Key Facts
- An increased risk of stroke events has been identified with the Pfizer COVID-19 bivalent vaccine, according to a joint statement from the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA).
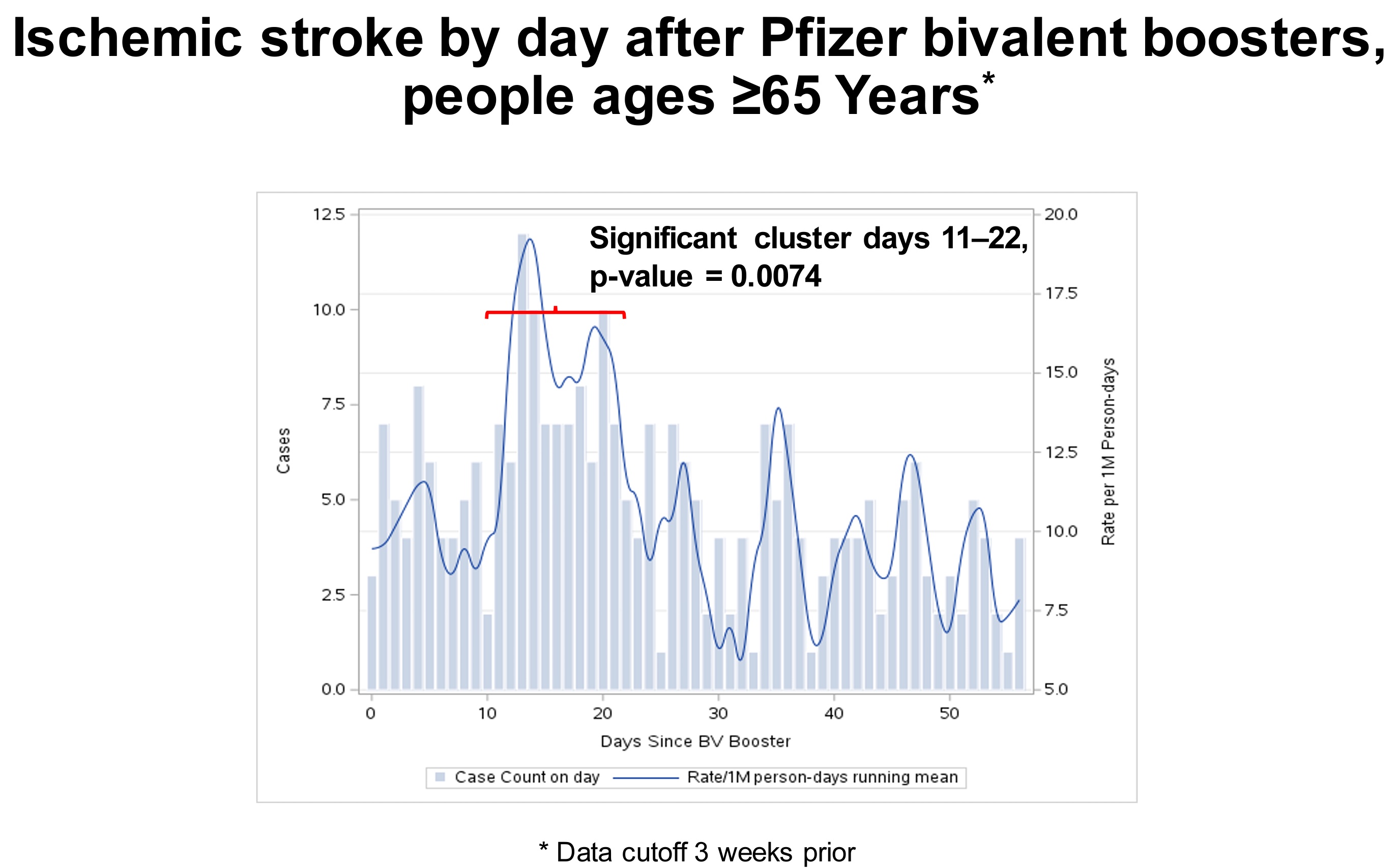
- The onset time in people aged 65 years and older was 1–21 days after the booster, with a significant cluster of events observed 11–21 days after the booster.
- Sixty-four percent had received the flu vaccine on the same day as the COVID-19 booster.
- The bivalent booster contains the code of the spike protein, contributing to the increased risk of blood clots. High-risk people should avoid the boosters.
- Solution: Remember the five “suddens” of stroke warning signs.
- Advice on preventing other risk factors of stroke is also provided in this paper.
On Jan. 13, 2023, the FDA and CDC issued a joint statement that a new “safety signal” for ischemic stroke had been detected in one of the agency’s vaccine safety surveillance systems.
The statement read, in part: “CDC’s Vaccine Safety Datalink (VSD), a near real-time surveillance system, met the statistical criteria to prompt additional investigation into whether there was a safety concern for ischemic stroke in people ages 65 and older who received the Pfizer-BioNTech COVID-19 vaccine bivalent.”
The VSD system monitors the electronic health records of 12.5 million Americans served by nine integrated health systems.
The CDC stated that no other safety databases had detected this signal (including the Medicare and Veterans Affairs data sets). Pfizer released a statement that it had not detected this signal in its databases, and no other countries have found a similar signal in their monitoring systems.
The clot risk appears to be greater on days 11–21 after receiving the booster, especially for those who received a high-dose or adjuvant flu vaccine on the same day.
A follow-up meeting was held on Jan. 26, 2023. Despite the identified risk, the CDC continues to recommend booster shots for all people over six months of age.
Increased Risk of Stroke Mostly Found 11 to 21 Days After Booster
The findings presented on Jan. 26, 2023, suggest that more stroke events occurred during days 1–21 post-vaccination than days 22–42 after receiving the shot.
People aged 65 or older who received the Pfizer bivalent booster experienced 130 events during the “risk interval” (1–21 days after the booster) and 92 events during the “comparison interval” (22–42 days after the booster). There was a 47 percent increased risk of ischemic stroke during 1-21 days post-booster, compared to those events occurring during 22-42 days post-booster, with a p = 0.005. In studies, when the P value is less than 0.05, it means the difference is statistically significant.
It is important to note that stroke events occurred throughout the entire 42-day follow-up period after the booster; a cluster of stroke events occurred between 11 and 21 days after receiving the booster.
In a preliminary review of 22 stroke cases in people 65 years or older on days 11–21 after receiving the booster, none of the individuals had a previous history of transient ischemic attack (TIA). Sixty-four percent received the flu vaccine on the same day as the COVID-19 booster (13 high-dose flu vaccines and one adjuvant flu vaccine).
Outcome data of these events shows that 59 percent of the people who experienced a TIA were discharged home, 18 percent were discharged with home health, nine percent were discharged to a skilled nursing facility, and 14 percent (three of the 22) died. The CDC notes that one death was likely related to a stroke.
No safety signal was detected in the VSD database for Moderna; however, the VAERS reported stroke cases related to the Moderna booster. The difference could be due to the number of booster doses administered for the two vaccines. Nearly twice as many Pfizer booster doses had been given as Moderna (549,943 vs. 285,706) as of Jan. 7, 2023.
As of Jan. 8, 2023, 40 ischemic stroke/transient ischemic attack cases after the bivalent COVID-19 mRNA vaccination were detected in the Vaccine Adverse Events Reporting System (VAERS). The median age was 74 years. Nineteen were males, and 21 were females. The median time to onset was four days. Twenty-five cases occurred after the Pfizer-BioNTech bivalent vaccine, and 15 occurred after the Moderna bivalent vaccine.
Receiving a Flu Shot on the Same Day as the Booster Increases Risk
VSD data analysis showed that three people experienced a stroke after receiving the Pfizer booster and a standard dose of flu vaccine on the same day. By contrast, 40 people who received the Pfizer booster and a high-dose or adjuvant flu vaccine on the same day experienced a stroke. Sixty older adults experienced a stroke after receiving only the COVID-19 booster.
Receiving a high dose or adjuvanted flu shot on the same day seemed to double the risk of stroke.
The spike protein in the SARS-CoV-2 virus can significantly increase the risk of arterial and venous clots. A database analysis of 48 million individuals in the United Kingdom found an increased risk of ischemic stroke, especially in the first weeks after COVID-19 infection.
The mRNA vaccine also produces the spike protein. The bivalent booster contains the code for two strains of the spike protein (original Wuhan strain and BA.4/BA.5).
Your blood contains platelets, which form clots to stop bleeding after an injury. The S1 unit of the spike protein hyperactivates these platelets. This can cause the blood to form tiny clots after infection or vaccination. These blockages in blood flow can cause problems throughout the body’s tissues and organs.
The flu shot increases the risk of stroke, possibly because the vaccine provokes an inflammatory response. This increases the risk of ischemic stroke, especially in people with pre-existing coagulation abnormalities. A report from Taiwan indicated that a 75-year-old male patient suffered posterior circulation ischemia after an influenza A/H1N1 vaccination.
Remember the ‘FAST’ Rule
Ischemic stroke occurs when a blood clot blocks or narrows an artery that leads to or is inside the brain. A blood clot often forms in arteries damaged by the buildup of plaques (atherosclerosis). It can occur in the carotid artery of the neck as well as in other arteries.
After vaccination—at a very rare rate—if an adverse stroke event does appear, what signs can alert you in time?
There are five “suddens” of stroke warning signs. If you observe one or more of these signs of a stroke, don’t wait; call a doctor or 911 immediately!
- Sudden numbness, weakness, or tingling of the face, arm, or leg, especially on one side of the body
- Sudden confusion, drowsiness, or trouble talking or understanding speech
- Sudden trouble seeing in one or both eyes, or double vision
- Sudden trouble walking, dizziness, or loss of balance or coordination
- Sudden severe headache, nausea, or vomiting with no known cause
Sometimes the signs may last only a few moments and then disappear. These episodes, known as transient ischemic attacks or TIAs, are called “mini-strokes.” Paying attention to them can be life-saving.
Remember the FAST (face, arm, speech, time) rule.
- F ace drooping? Can’t smile
- A rm weakness? Can’t raise above head
- S peech difficulty? Can’t repeat simple nursery rhyme
- T ime to call 911.
One or more of these signs—face weakness, arm weakness, and speech difficulty—are present in 88 percent of all strokes and TIAs. Getting to an emergency room quickly can save your life or the life of a loved one.
An intravenous injection of recombinant tissue plasminogen activator (rtPA) is the gold standard treatment for selected patients with ischemic stroke. An injection of TPA is usually given through a vein in the arm within the first three hours after a stroke.
Arriving at an emergency room as quickly as possible after noticing symptoms is critical to reducing the odds of disability. A successful rescue of stroke patients includes early identification of signs of stroke and medical care within the first hour of acute stroke.
Recommendations on Vaccinations
It may not be advisable for individuals vaccinated against COVID-19 and who experienced a stroke to take extra COVID-19 jabs such as boosters.
For now, this safety signal looks like a worrisome association with vaccination. Elderly individuals at high risk for severe COVID-19 should check with their physicians for the most appropriate guidance tailored to their risks, given that COVID-19 also increases the risk of stroke and other cardiovascular events for months after infection.
Carefully monitor individuals who received the COVID-19 vaccine or flu vaccine, especially those with high ischemic stroke risk.
A few sensible recommendations worth discussing with your physician include:
- Consider separating the bivalent booster from other routine immunizations until more data has been collected; and
- Wait several months after COVID-19 infection before getting a booster so that the increased risk of cardiovascular events following infection diminishes before introducing a new risk.
Lifestyle Tips to Prevent Stroke
There are many natural ways to support your body in breaking down the spike protein after vaccination or infection. It is vital to keep moving, drink plenty of fluids, and make deliberate dietary choices to increase antioxidant and antiplatelet nutrients.
Stroke as an adverse effect of vaccination won’t happen to everyone, and this means there are things we can do to reduce the risk.
Many of the risk factors of stroke are shared with cardiovascular diseases or heart attacks, as strokes and heart attacks are both associated with blood vessel problems. The risk of a stroke increases with age. Smoking, high blood pressure, high cholesterol, obesity, and diabetes also increase the risk of stroke.
Lifestyle modifications are recommended for everyone, not just those at a high risk of stroke. We hear these recommendations often because they are proven to help maintain good health. Regular physical activity is essential. Maintaining a healthy diet and getting good-quality sleep set the foundation for feeling well. Avoid nicotine (smoking or vaping) and limit alcohol consumption. These steps help control your blood pressure, glucose, and lipid levels.
There are a few tips that may help reduce the risk of stroke. Start them now and make improvements to your life:
1. Spend some time inside the comforter or quilt in the morning before getting out of bed. As blood circulation is slow during sleep, taking 20 minutes of warm-up time to activate the blood throughout the body would speed up blood circulation and reduce the risk of stroke.
2. Drink a glass of warm water after getting up. An eight-ounce glass of warm water helps hydrate your body and can dilute the blood to promote blood circulation. Warm water can lower the risk of myocardial and cerebral stroke. Avoid cold water, as it can make your vessels contract rather than dilate.
3. Eating a banana for breakfast will facilitate a bowel movement in the morning. Don’t push too hard in the effort to eliminate, as pushing can increase blood pressure. Healthy bowel movements can help expel toxins and waste. Of course, our bodies will appreciate it if we can do this daily.
4. Avoid eating irritating foods such as strong coffee, alcohol, chili, or pepper. They may induce the contraction of blood vessels and increase blood pressure.
5. Avoid high-salt, deep-fried foods and choose healthy, organic, whole food as much as possible. The latter type of food typically contains large quantities of antioxidants and is beneficial for blood vessels and metabolism.
6. Do regular gentle daily exercises, including slow walking, Qigong, Taiji, or sitting meditation if you can cross your legs. Many research studies demonstrate that once we have such long-term healthy habits, we can elevate our health level holistically.
Take Mind-body Approaches to Preventing Stroke
Humans are not just physical creatures. Human beings are holistic, i.e., we are made up of physical, emotional, and mental aspects. Try to identify and modify psychosocial and emotional stressors.
Researchers found that type A behavior has been associated with an increased risk of stroke. High conscientiousness was found to be protective against stroke-related mortality.
A cross-sectional study examined significant stroke risk factors of hypertension, diabetes, and obesity, as well as personality and emotions. Among personality traits, high agreeableness was associated with reduced systolic hypertension (p = 0.039) and diabetes (p = 0.010). Anger was associated with increased diabetes (p = 0.009), while fear was associated with increased obesity (p = 0.024).
A high level of agreeableness appears protective against hypertension and diabetes, whereas anger and fear may predispose individuals to diabetes and obesity. The same trends should apply to the association with stroke as well.
You have a great deal of influence over your health. Why not begin making positive changes today?
