
In 2019, the World Health Organization (WHO) proposed 10 threats to global health, such as air pollution, non-communicable diseases, global influenza pandemic, Ebola and other high-threat pathogens, weak primary health care, and HIV. Among them, vaccine hesitancy was also mentioned, which many people might find surprising.
The elevation of this issue to a global health threat is a rather political approach. From this perspective, it should not be acceptable to the public. Just as consumers evaluate the quality of the products they purchase, people want to know the vaccines they are getting are good in quality and effective. If a vaccine is proven to be effective while there are minimal side effects, most people wouldn’t hesitate to get vaccinated.
Furthermore, vaccination is just one of the preventive measures aimed at protecting the vaccine recipients against certain diseases. And vaccine’s protection effects depend on the functional immune system in the vaccinated people’s bodies. There are many other ways to achieve the same outcomes, such as boosting the individuals’ innate immunity. Also, for some diseases, there are effective medications to cure the patients, alleviate their symptoms, or prevent critical illness.
The term “vaccine hesitancy” is not scientific per se. Rather, it is a political term. In fact, it has become a label that can be used to attack people. In many cases, people who are described as “vaccine hesitant” are also labeled as “anti-science.” This is irrational and shouldn’t be promoted, especially by such an authoritative international health organization as the WHO. This is because the qualities of different vaccines vary greatly. Labeling people “vaccine hesitant” is a practice to violate their right to self-determination. Therefore, people should question whether there are political operations or interest groups behind the campaigns to attack people for “vaccine hesitancy.”
One such example is the WHO’s promotion of the human papillomavirus (HPV) vaccine, in the name of eliminating cervical cancer on a global scale. However, prior to the development of cervical cancer, there are already pre-cancerous cells in many females, which can be caused by various internal mechanisms of the human body. Vaccination alone cannot prevent the development of all cervical cancer cases. Therefore, the WHO’s proposal to eliminate cervical cancer through HPV vaccination is unscientific and sounds like a marketing campaign for the vaccine products. The HPV vaccines would reduce the occurrence of cervical cancer, but cannot eliminate it.
Flu Vaccines Have Varying Effects on the Immune Responses of Different Age Groups
Currently, the most commonly used production method of influenza vaccines is the egg-based approach, in which flu viruses grow and replicate themselves. They are then isolated, purified, and inactivated, before being added to the formulation to produce vaccines. Although cost-effective, this method is prone to mutations, which can lower the vaccines’ effectiveness and cause potential problems, such as weakening the vaccine recipients’ immune system.
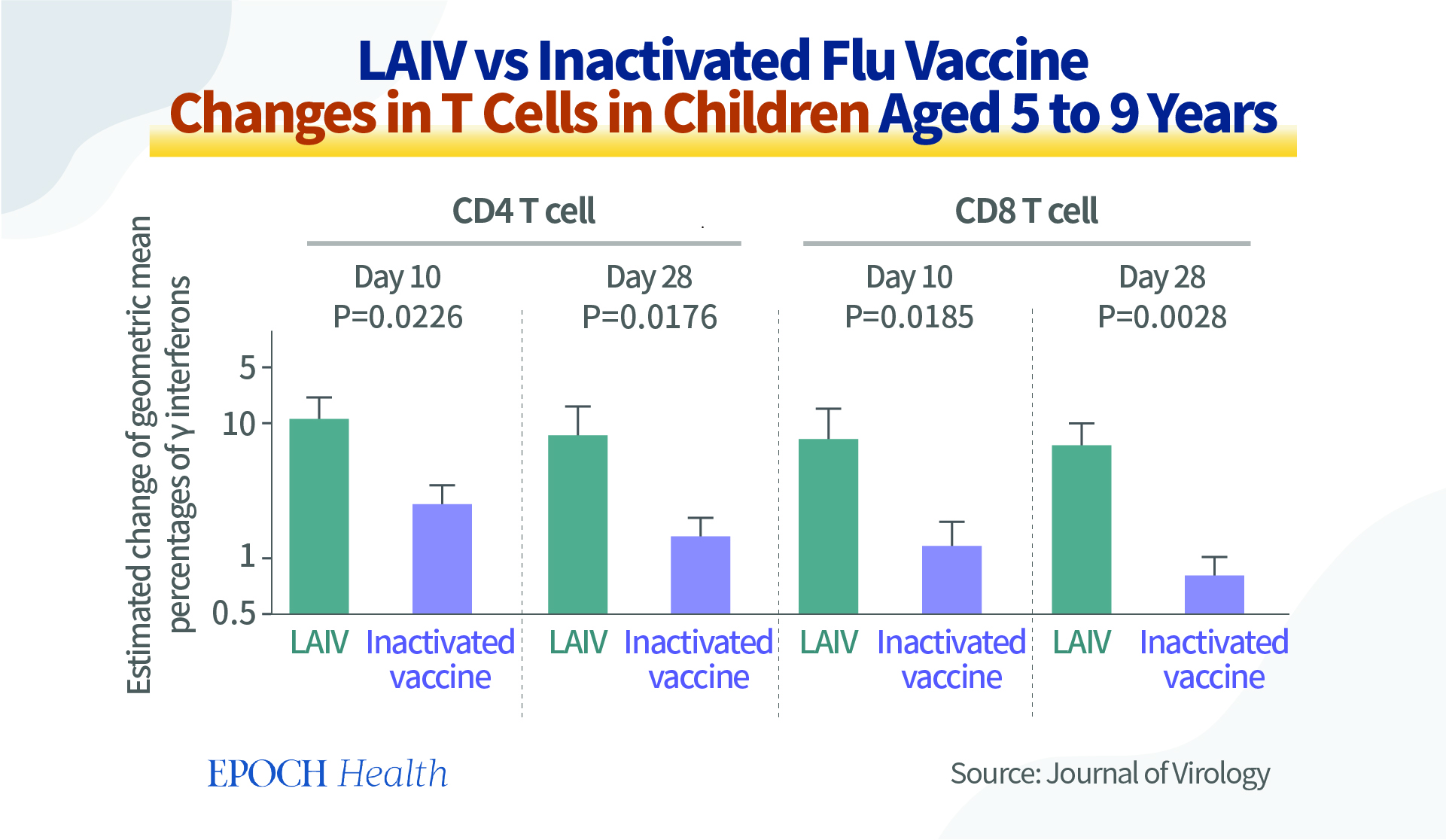
When implementing flu vaccines, the more responses from T cells and B cells, the better. From the graph below, we can see that among children aged 5 to 9, in terms of T-cell response stimulation, inactivated flu vaccines are less effective than live attenuated influenza vaccines (LAIVs) (pdf).
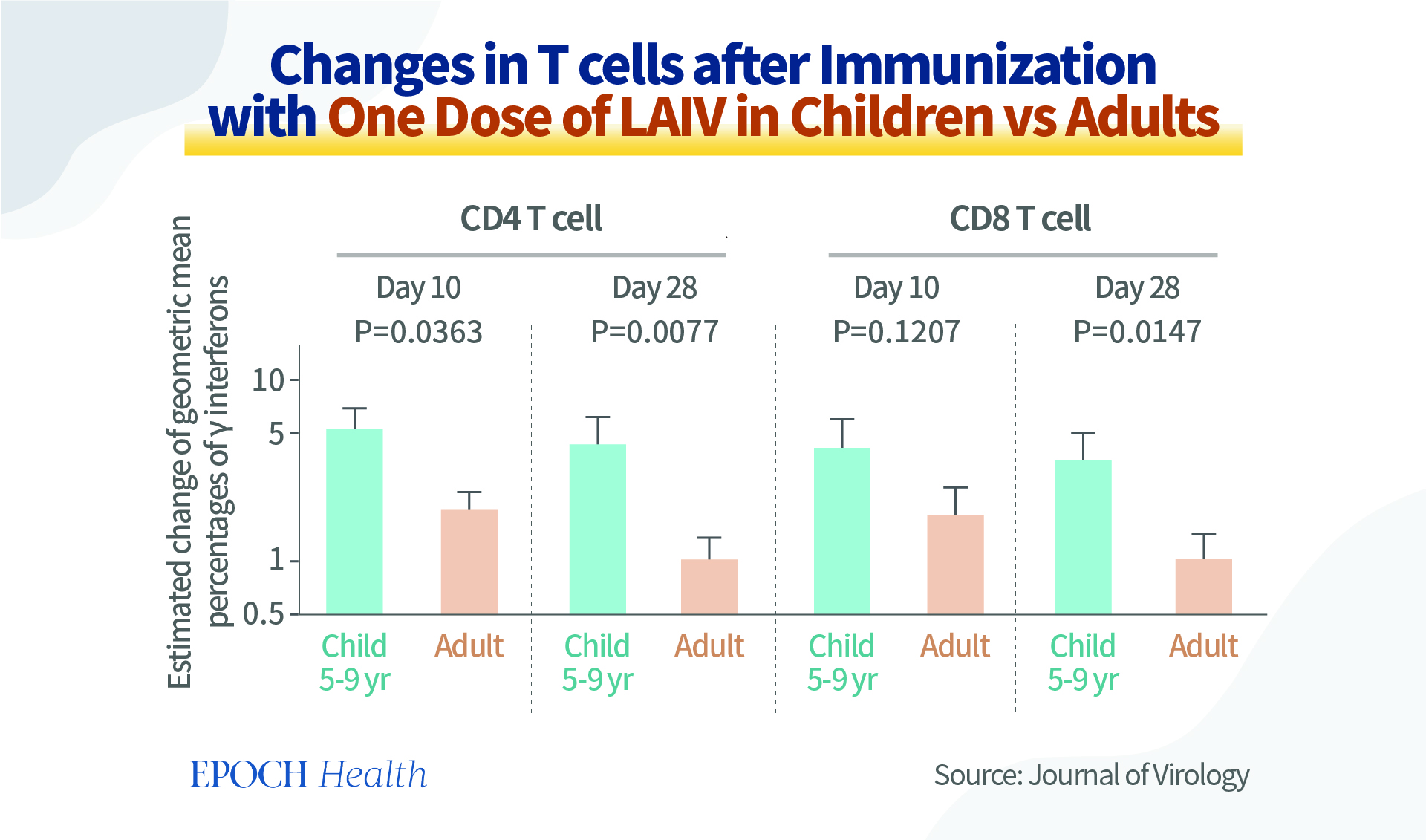
Furthermore, vaccines are not a panacea that works for everyone or every age group. This graph shows the changes in the T cells of children and adults after their immunization with one dose of LAIV. We can see that although the same type of flu vaccines were administered, in terms of T cell response, the vaccines are more effective in children aged 5 to 9 years than in adults. In addition, different vaccine platforms also have different effects on vaccine recipients.
Therefore, we can conclude that these flu vaccines have varying effects on different age groups. The same vaccines may not have the same protection for everyone, as individual factors such as age, gender, body mass index (BMI), and response to vaccines are also involved, and they may vary greatly among different populations. So, when designing vaccination policies, there should be some adjustment for different age groups. This also further illustrates our points earlier that people should have the self-determination for vaccinations based on their own individual factors, such as the age factor here.
New Generation of Flu Vaccines Will Also Have Mutations and Challenges
Although LAIVs are more effective than inactivated flu vaccines when providing protection, they are not as widely promoted as inactivated vaccines, due to their side effects. Therefore, the next generation vaccines are expected to have better stimulation of T cell responses through new technologies, such as the DNA recombinant technology. One example of a next generation flu vaccine is Wyeth/IL-15/5Flu, which is a T cell-activating vaccine based on the H5N1 flu strain and produced by the pharmaceutical company Wyeth.
However, this T cell-activating vaccine induces a higher incidence and degree of mutation on the influenza A virus genome. That is, even if the virus strains used in the production of the vaccine are not grown from eggs, there will still be mutations at important hemagglutinin-receptor binding sites. For example, in the flu virus strain used in Wyeth/IL-15/5Flu vaccine production, it was found that the mutation at position 34 (involved in receptor binding) in HA protein is 10 times higher than virus strains used for inactivated vaccines.
For instance, when producing these new vaccines, once the mutation-prone virus hemagglutinin’s head domain is removed, its hemagglutinin (HA) stem region, which has a relatively low mutation frequency, will now mutate more. And beneficial adaptation mutations on the polymerase basic 2 (PB2) gene/protein can occur, as the virus adapts to the new production method and environment. As breakthroughs are produced, the stem, which was previously not prone to mutations, would also mutate.
In addition to the mutations brought about by the immune environment, the vaccine companies would also deliberately select the fast-growing strains of influenza virus. This is because for high volume virus production, the choice of virus strains with higher reproduction efficiency is also important. So, it is necessary for vaccine companies to select strains that reproduce fast, in order to grow more viruses with fewer resources.
During this virus strain screening process, mutations concerning gene segments such as the viral enzymes PB1 and PB2 are introduced, and this changes the strains’ replication capability. Also, many of the new generation vaccines are in Vero cells, which are a lineage of monkey kidney epithelial cells and the most popular cell lineage for manufacturing human vaccines. However, Vero cells are not human cells. The virus still needs to adapt to a different host when using Vero cells.
The Impact of Annual Vaccination on the Human Immune System and the Flu Virus
In the 1970s, T.W. Hoskins and colleagues observed a phenomenon in a British boarding school for the first time. That is, flu vaccination in prior influenza seasons can reduce the effectiveness of the vaccine in the current season. This phenomenon, known as the “Hoskins effect,” has also been identified by some other studies.
Although academics have been exploring the “Hoskins effect” for decades and scratching their heads over this phenomenon, the general public is not aware of this issue.
Many people believe that the benefits of flu vaccination outweigh its drawbacks. This is why they are promoting the implementation of flu vaccines. Although there have always been questions about the effectiveness of flu vaccines, there haven’t been any large-scale studies on this issue so far.
Currently, the Centers for Disease Control and Prevention (CDC) recommends people over the age of 6 months to receive seasonal flu vaccines. However, what are the impact of annual flu vaccination on our immunity?
According to the journal Frontiers in Immunology, a human cohort vaccine study has been conducted since the 2016-2017 flu season with adult (over the age of 18) and teenage (12 to 18 years old) participants, who are vaccinated annually against the seasonal flu. Every flu season, the subjects’ sera samples and personal information are collected and analyzed at the University of Georgia.
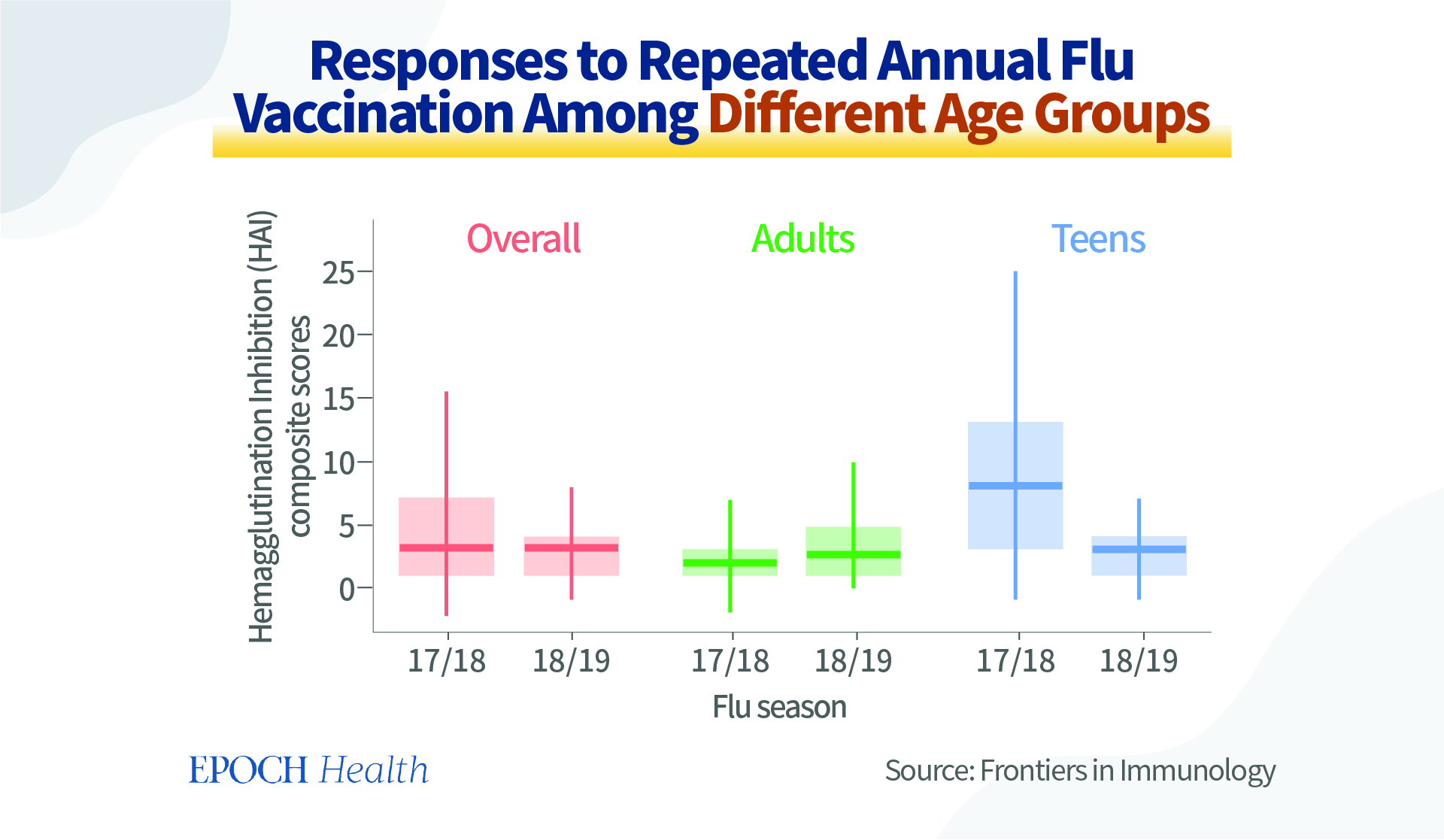
Their immune responses to repeated annual influenza vaccination is tested by hemagglutination Inhibition (HAI) composite scores. The participants are enrolled in early September every year, without having received the seasonal flu vaccine. In the teenage participant group, during the 2017-2018 flu season, the hemagglutination inhibition was relatively adequate. However, the inhibition came down in the following flu season. The same phenomenon took place in the adult group, as well.
It can be interpreted that at the beginning of the 2017-2018 flu season, the participants were not vaccinated, and the flu vaccine later provided them with useful protection. However, in the subsequent 2018-2019 flu season, with repeated flu vaccination, the protection offered by the vaccine actually decreased. It has also been observed that the vaccine had become less and less effective among the repeatedly vaccinated participants.
Overall, the HAI composite scores declined significantly from one flu season to the next in teenagers, but somehow remained steady in adult participants. In addition, a comparison of the mean HAI composite scores of prior vaccinated teens and those newly enrolled in the 2018-2019 flu season implies that repeated annual vaccination resulted in reduced immune responses.
Therefore, repeated vaccination strains are associated with reduced boosting of immune responses and thus protection.
The annual flu vaccine contains four different virus strains. It was discovered that if the virus is the same, to very similar year to year, the decline in immune response would be more obvious if the vaccine had been given continuously year to year. In addition, if there is a change in the choice of virus strains between seasons, the vaccine’s protection effect would be better. This may be because the immune system has been fatigued by the repeated vaccination.
The immune system may use the immunological memory based on the previous vaccination when a second slightly different vaccine is administered, leaving the immune system stuck with its first immune responses and unable to generate more effective responses to the second vaccination. However, as flu viral strains change from year to year, the antigens in the vaccine are also adjusted. There has been no tracking of the immune fatigue associated with a particular strain of virus. And the specific mechanism of this phenomenon has not been studied in particular detail.
In addition, repeated vaccination also forces the virus to undergo mutation, as it guides the virus to develop in a certain direction, as it screens the virus strains. This is called immune escape.
During the natural evolution process, pathogens experience random mutations that change their antigens. Therefore, the vaccine loses its effectiveness against the mutated pathogens. Nevertheless, during the vaccine-driven evolution process, after the vaccine is administered, certain pathogens die, and the surviving ones replicate themselves. After several rounds of repeated vaccination, the surviving pathogens would have gone through several rounds of screening, and the vaccine then has less effect on them. And eventually, vaccine-escape mutants will be screened out.
Vaccine escape does not just occur for flu vaccines. There are many examples for other bacteria vaccines. Lessons were not rare.
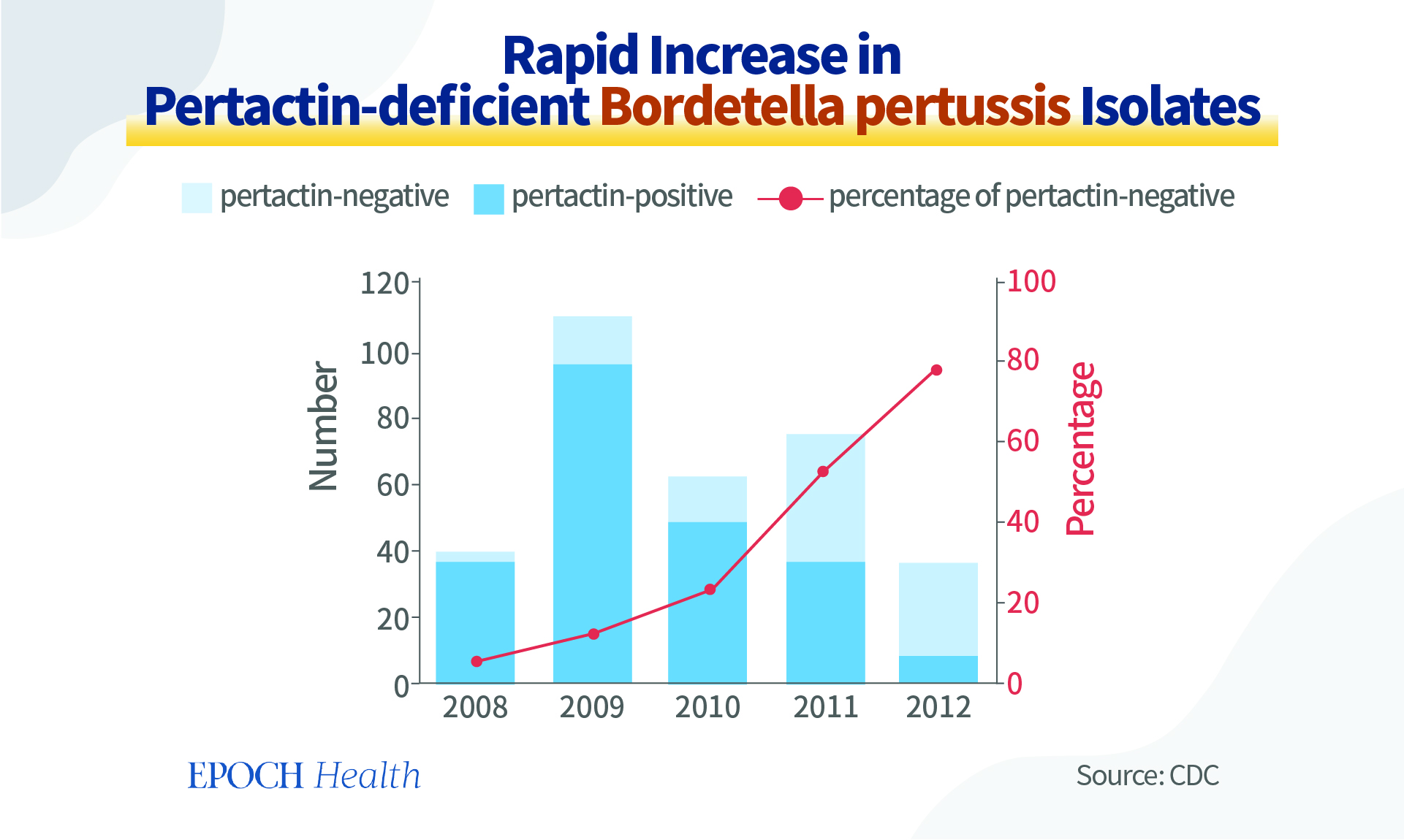
For example, Bordetella pertussis is the bacterium causing pertussis (whooping cough). As the design of the vaccine against Bordetella pertussis was targeting one of its surface-associated proteins called pertactin, through self-screening, more and more pertactin-negative bacterial isolates were replicating themselves more than the other ones.
This immune escape phenomenon may explain the fact that since the 2009-2010 flu season, the effectiveness of the flu vaccines has been below 50 percent most years.
Do Flu Shots Reduce the Rate of Severe Illness?
Many people get the annual flu jabs, because they believe that they can prevent severe illness. However, the results of a Japanese study may disappoint. This study, published in the journal Vaccine in 2014, shows that flu vaccination doesn’t reduce the risk of subsequent hospitalization or prevent severe illness.
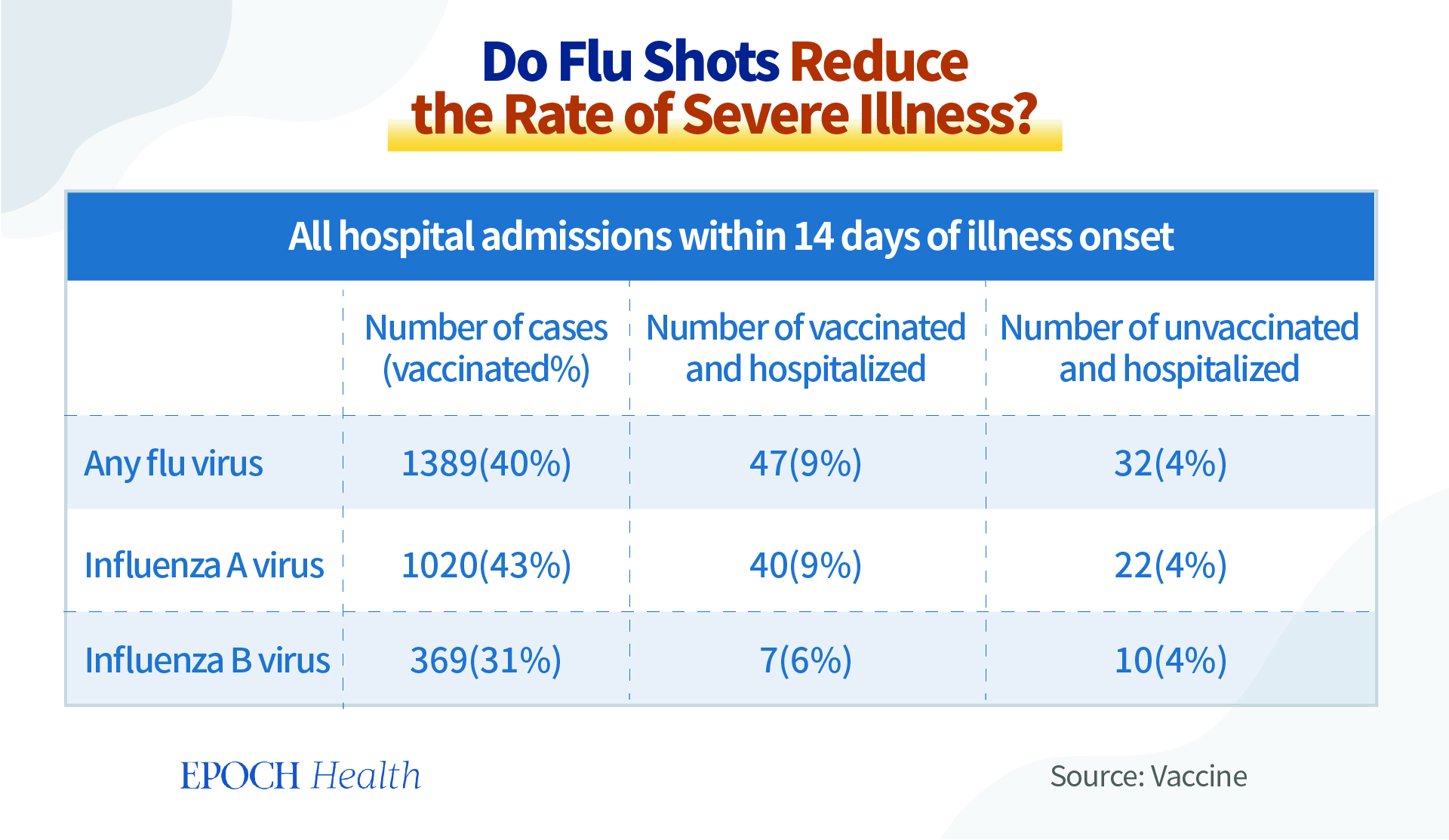
As shown in the table, within 14 days of flu infection, around 40 percent of people who had previously been vaccinated with the flu vaccine were infected with the flu virus. And the percentage of cases in which the individuals got vaccinated and became hospitalized was 9 percent, while this figure was 4 percent for the hospitalized patients who were unvaccinated. Therefore, the flu vaccine doesn’t always reduce disease severity or prevent critical illness as the general public believes, a belief driven by the annual flu vaccination campaigns.
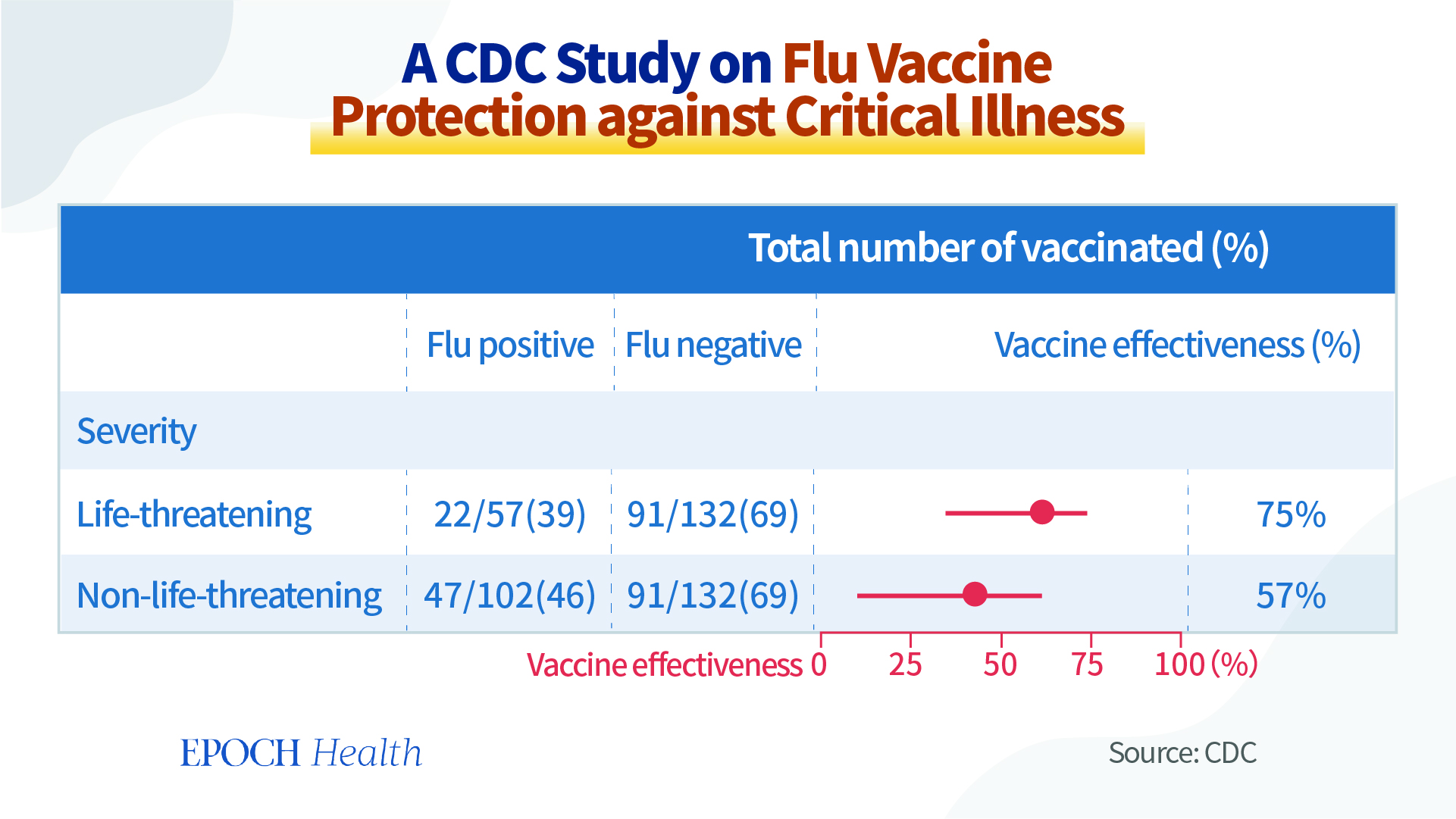
The CDC also conducted a study on flu-caused critical illness among a vaccinated population recently. The patients with life-threatening illness included those who used invasive ventilation, vasopressor, dialysis, and cardiopulmonary resuscitation.
According to this study, the flu vaccine was effective in 75 percent of the cases with life-threatening illness and in 57 percent of the cases with non-life-threatening illness.
However, this study is not very rigorous, as its sample size is very small. More importantly, the factor of underlying medical conditions was not included in the evaluation of the patients’ disease severity, as many of them already had respiratory, cardiovascular, and/or neurological conditions prior to flu infection. The data of disease severity was not stratified based on different types and degrees of underlying medical conditions. The data shown in this paper only pointed out how many people, whether vaccinated or not, have underlying medical conditions. Therefore, this study is very biased and it draws more conclusions than its data can suggest.
So, in summary, objective evaluation of vaccine efficacy and safety are critical to provide unbiased information to the public. And international organizations or health regulators should avoid politicizing the people who carefully evaluate of their choice of vaccinations. “Vaccine Hesitancy” is a political label that should be abandoned by health agencies and international organizations like WHO.
