
Several pathogenic microbes were identified and quantified on masks worn during the pandemic, according to a Japanese study that was published in Scientific Reports.
The study is one of the first to address the probable hygiene issues caused by bacterial and fungal growth on masks worn daily in the community.
“Since masks can be a direct source of infection to the respiratory tract, digestive tract, and skin, it is crucial to maintain their hygiene to prevent bacterial and fungal infections that can exacerbate COVID-19,” the authors wrote.
The study involved 109 participants aged 21 to 22 years who were asked about the type and duration of mask used and their lifestyle habits. Bacteria and fungi were collected from the three types of masks—gauze, polyurethane, and non-woven—worn between September and October 2020.
The researchers found that the face side of the masks had more bacteria, whereas the outer side of the masks contained more fungi.
In addition, longer use of the mask resulted in an increase in fungi but not in bacteria because “fungi and their spores are resistant to drying, they can survive under the condition where masks dry out.”
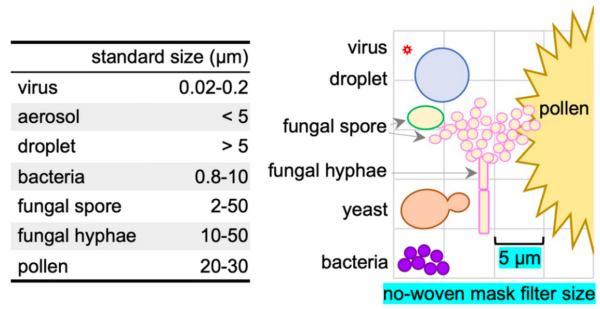
Non-woven masks were found to have fewer fungal colony counts on the outer side compared to the other two mask types. Non-woven masks have three layers, two-layer fabric with a non-woven middle layer filter.
Researchers said they were surprised to find that there were no significant differences in the numbers of bacteria or fungi on washable or reusable masks that had been washed.
“The proper cleaning method for cotton face masks has been recommended to reduce the microbial load on the masks,” the authors wrote. “However, in the current experiments, we did not find significant differences in bacterial or fungal colony numbers on the masks based on washing.”
Lifestyle Habits
The researchers also examined whether certain lifestyle habits such as gargling, consumption of natto, and use of the different modes of transportation—public transportation, personal vehicle, and walking or biking— had any effect on the microbial counts on the masks.
“We found no differences in the bacterial or fungal colony counts on both sides of the masks among the three transportation systems,” the authors wrote.
There were also no differences in microbial counts on masks of participants who gargled once a day. Gargling is a Japanese custom believed to prevent respiratory infections. The practice is often recommended by the Japanese health authority alongside hand washing as a preventative measure against influenza.
A study from Penn State College of Medicine published in the Journal of Medical Virology in September 2020 found that several types of mouthwash and nasal rinses were effective at neutralizing human coronaviruses, suggesting that the products may have the potential to lessen the amount of SARS-CoV-2 load, or the amount of virus inside the mouth. SARS-CoV-2 is the virus that causes COVID-19.
A small pilot study is currently being conducted by the University of California, San Francisco on whether gargling with certain mouthwash or gargling solutions will reduce viral load in patients diagnosed with COVID-19. The study is expected to complete this September.
Gargling with antiseptic mouthwashes is part of the Front Line COVID-19 Critical Care (FLCCC) Alliance’s protocol for “both chronic (ongoing) prevention as well as to avoid getting sick” after an individual has been exposed to the virus.
FLCCC Alliance is a nonprofit organization consisting of critical care specialists who’ve dedicated their time to developing treatment protocols to “prevent the transmission of COVID-19 and to improve the outcomes for patients ill with the disease.”
As for the consumption of natto, soybeans that are fermented with a bacterium called bacillus subtillis or B. subtilliss, the researchers said that the participants who consumed the sticky soybeans, “had a significantly higher incidence of large white B. subtillis colonies on both sides of the masks than those who did not.”
B. subtillis is a bacterium found in soil, water, decomposing plant residue, and air. It is used for “industrial production of proteases, amylases, antibiotics, and specialty chemicals” and is “not considered pathogenic or toxigenic to humans, animals, or plants,” according to the U.S. Environmental Protection Agency (pdf).
Pathogenic Microbes
While most of the bacteria and fungi cultured from the masks were not harmful to humans, some were opportunist pathogens, while others were found to cause diseases like bacteria that cause food poisoning and staph infections, and a fungus that causes ringworm, athlete’s foot, and jock itch.
From their findings, the authors of the study suggest that people with a weakened immune system should “avoid repeated use of masks to prevent microbial infection.”
The CDC says that immunocompromised people or those at high risk for severe disease should wear a mask or respirator when there is a high community level of COVID-19.
The health agency did not respond to The Epoch Times’ request for comment on the findings of the Japanese study.
Supporters of universal masking during the pandemic say that masks help to prevent or reduce transmission of SARS-CoV-2 infection.
Scientific Evidence
Epidemiologist and researcher Dr. Paul Alexander disagree. He says that there are over 150 studies and articles that conclude cloth and surgical masks are not effective in slowing the spread of COVID-19 and does more harm.
“To date, the evidence has been stable and clear that masks do not work to control the virus and they can be harmful and especially to children,” Alexander wrote in a February op-ed for The Epoch Times.
In a critical review (pdf) of cloth masks used during the pandemic, the authors stated that evidence does not support community masking with cloth masks to limit the spread of the virus.
“The available clinical evidence of facemask efficacy is of low quality and the best available clinical evidence has mostly failed to show efficacy, with fourteen of sixteen identified randomized controlled trials comparing face masks to no mask controls failing to find statistically significant benefit in the intent-to-treat populations,” the authors wrote.
“Although weak evidence should not preclude precautionary actions in the face of unprecedented events such as the COVID-19 pandemic, ethical principles require that the strength of the evidence and best estimates of amount of benefit be truthfully communicated to the public,” they added.
Prior to the pandemic, researchers conducted a small randomized controlled study in 2008 among health care workers in Japan to examine whether surgical masks reduced the incidence of the common cold.
They found that participants in the mask group “were significantly more likely to experience headache during the study period” and concluded that “face mask use in health care workers has not been demonstrated to provide benefit in terms of cold symptoms or getting colds.”
