Ivermectin is an anti-parasitic agent that has gained attention as a potential COVID-19 therapeutic. It is a compound of the type Avermectin, which is a fermented by-product of Streptomyces avermitilis. Bifidobacterium is a member of the same phylum as Streptomyces spp., suggesting it may have a symbiotic relation with Streptomyces.
Decreased Bifidobacterium levels are observed in COVID-19 susceptibility states, including old age, autoimmune disorder, and obesity. We hypothesize that Ivermectin, as a by-product of Streptomyces fermentation, is capable of feeding Bifidobacterium, thereby possibly preventing against COVID-19 susceptibilities.
Moreover, Bifidobacterium may be capable of boosting natural immunity, offering more direct COVID-19 protection. These data concord with our study, as well as others, that show Ivermectin protects against COVID-19.
Introduction
SARS-CoV-2 infection has been a global pandemic affecting the world for the last 2+ years. Symptoms include fever, cough, shortness of breath, GI issues, potential pneumonia, and other less common ones, including oral symptoms (Khodavirdipour et al., 2021a; Sharma et al., 2021). Current treatments for SARS-CoV-2 include remdesivir, paxlovid, hydroxychloroquine, nucleoside analogs, antibodies, antibiotics, herbal medicines, tocilizumab, anti-inflammatory drugs (e.g., steroids), and ivermectin (IVM) (Gavriatopoulou et al., 2021). Vaccines have been distributed widely for SAR-CoV-2 infection (Khodavirdipour et al., 2020; Joshi et al., 2021) prevention. In addition to standard nasopharyngeal tests, CRISPR-based methods (Khodavirdipour et al., 2021c) have been used or proposed for SARS-CoV-2 infection testing. Recent mutations have been making SARS-CoV-2 infection more contagious and with a higher rate of Khodavirdipour et al. (2021b) infection. Nonetheless, the pandemic has continued for over 2 years, and a better understanding of all possible therapeutics is essential.
Severity of SARS-CoV-2 has been associated with lower levels of Bifidobacterium (Tao et al., 2020; Xu et al., 2020; Reinold et al., 2021; Yeoh et al., 2021; Zuo et al., 2021; Hazan et al., 2022b). Probiotics have been hypothesized and tested with success for improving SARS-CoV-2 symptoms (Bozkurt and Quigley, 2020; Bozkurt and Bilen, 2021; Khaled, 2021; Khodavirdipour, 2021; Gutiérrez-Castrellón et al., 2022; Khodavirdipour et al., 2022), and they are often enhanced by use with prebiotics (Markowiak and Śliżewska, 2017). Thus, we sought to find medications that increase the level of beneficial gut bacteria, i.e., have a prebiotic effect.
Ivermectin Has Been Shown to Effectively Treat SARS-CoV-2 Infection
Over 40 peer-reviewed studies (Table 1) have demonstrated studies on the effectiveness of IVM in SARS-CoV-2 infection (Alam et al., 2020; Khan et al., 2020; Kishoria et al., 2020; Reaz et al., 2020; Abd-Elsalam et al., 2021; Ahmed et al., 2021; Ahsan et al., 2021; Aref et al., 2021; Behera et al., 2021; Cadegiani et al., 2021; Chaccour et al., 2021; Chahla et al., 2021; Chowdhury et al., 2021; Elalfy et al., 2021; Faisal et al., 2021; Ferreira et al., 2021; Hellwig and Maia, 2021; Krolewiecki et al., 2021; Lima-Morales et al., 2021; López-Medina et al., 2021; Mohan et al., 2021; Morgenstern et al., 2021; Mukarram, 2021; Okumuş et al., 2021; Podder et al., 2021; Rajter et al., 2021; Ravikirti et al., 2021; Rezk et al., 2021; Seet et al., 2021; Shahbaznejad et al., 2021; Shoumann et al., 2021; Abbas et al., 2022; Ascencio-Montiel et al., 2022; Babalola et al., 2022; Beltran Gonzalez et al., 2022; Buonfrate et al., 2022; Hazan et al., 2022a; Kerr et al., 2022; Lim et al., 2022; Mayer et al., 2022; Mustafa et al., 2022; Ozer et al., 2022; Reis et al., 2022; Shimizu et al., 2022; Zubair et al., 2022), with over 80% of studies showing positive outcomes with IVM treatment. Overall, IVM has shown 60–85% improvement in outcomes, including mortality, ventilation, recovery, clearance, and hospital/ICU admissions. The effectiveness could be particularly strong at high doses (Krolewiecki et al., 2021; Buonfrate et al., 2022; Mayer et al., 2022) and for severe SARS-CoV-2 infection (Beltran Gonzalez et al., 2022; Hazan et al., 2022a; Zubair et al., 2022), and one must consider that the effective dose is very affected by food co-administration (Food and Drug Administration, 2022). Thus, there is a tremendous need to ascertain, not whether but how IVM is ideally applied for SARS-CoV-2 infection.
Table 1
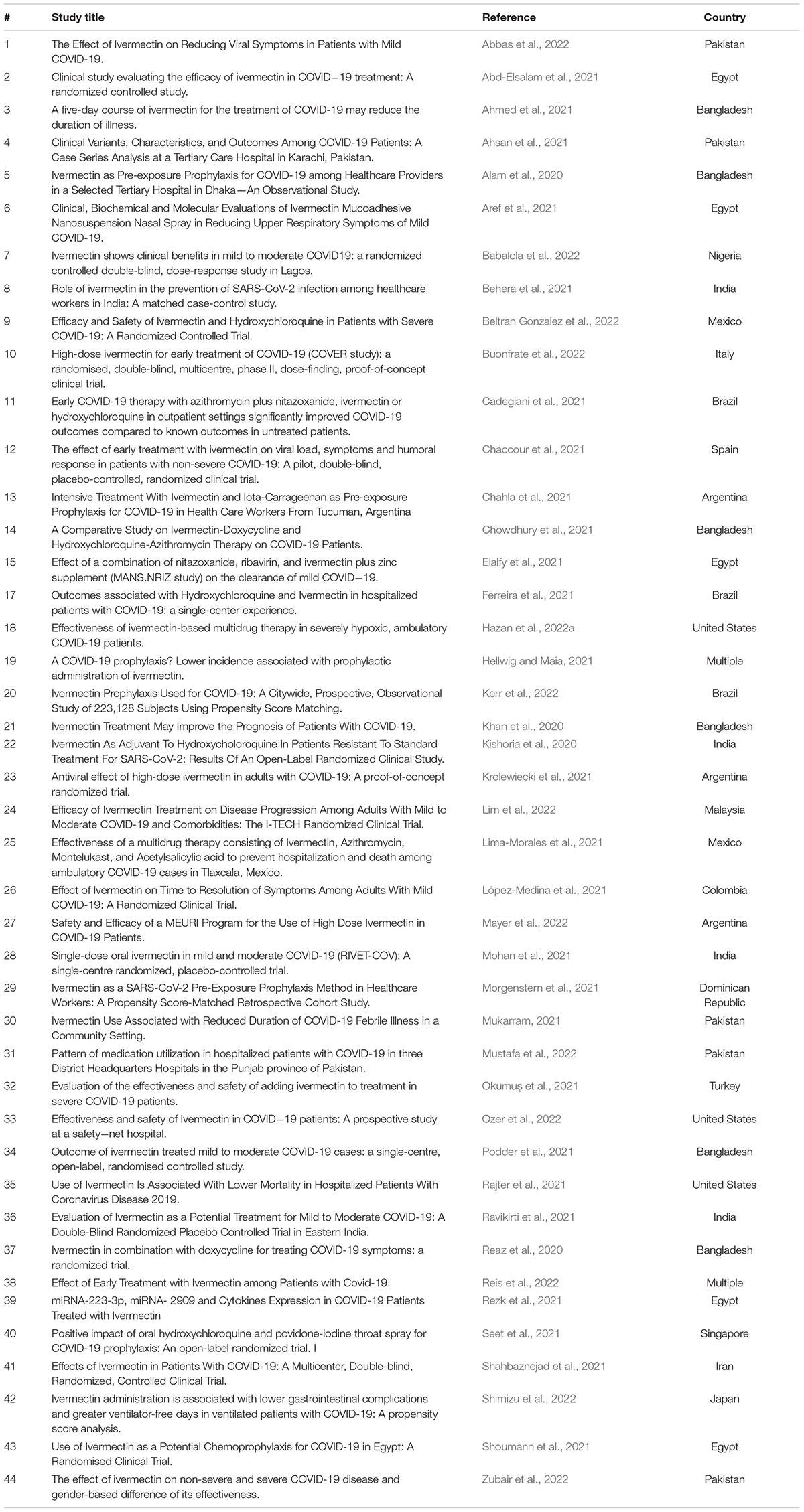
TABLE 1. Peer-reviewed studies regarding efficacy of Ivermectin in SARS-CoV-2 infection.
The demonstrated effectiveness of IVM in SARS-CoV-2 cannot be ignored. An important step toward refining our understanding of when and how IVM is successful is that we need to understand all potential mechanisms for IVM against SARS-CoV-2 infection. The purpose of this study is to describe a novel hypothesis for IVM action against SARS-CoV-2 for consideration by the scientific community. While there is limited published evidence for this—as of yet theoretical description—we are soon to publish data showing in vivo administration of IVM increases-relative abundance of Bifidobacterium.
Background to the Hypothesis
IVM discovery was awarded the Nobel prize (Molyneux and Ward, 2015), 35 years post-discovery, for its game-changing impact on the field of antiparasitic agents. IVM is approved by the Food and Drug Administration for treating parasitic infections and comes from the class compounds called macrocyclic lactones, specifically Avermectins. Avermectins are found naturally as a fermentation product of a strain of Streptomyces avermitilis (Laing et al., 2017). While IVM’s mechanisms of action as an anti-parasitic agent are well-established (Ômura and Crump, 2014), its potential in fighting viral infectious disease, including possibly SARS-CoV-2 infection, remains poorly understood.
Streptomyces spp. belong to the same phylum as a critically important constituent of the gut microbiome and common ingredient of probiotics, Bifidobacterium. Bifidobacterium abundance is known to decrease in SARS-CoV-2-infected subjects, as seen in ours and other studies (Tao et al., 2020; Xu et al., 2020; Reinold et al., 2021; Yeoh et al., 2021; Zuo et al., 2021; Hazan et al., 2022b). We have anecdotally observed, through our clinical experiences pre and post Fecal Microbiota Transplant, that certain bacteria in the same phylum may be able to replace each other’s function. Thus, we hypothesized Streptomyces spp. may replace loss of Bifidobacterium.
Bifidobacterium spp. are microaerotolerant anaerobes that degrade monosaccharides, such as glucose and fructose, via the bifid shunt, or the fructose-6-phosphate phosphoketolase pathway and produce more ATP than traditional fermentative pathways (De Vuyst et al., 2014). Bifidobacterium spp. also symbiotically feed other gut microbes via their metabolic by-products and end-products, which, in turn, enhance butyrate production and reduce inflammation (De Vuyst et al., 2014). Streptomycesspp., too, are frequently found in symbiotic relations with other bacteria (Seipke et al., 2012). Thus, it is possible for a symbiotic relation between Streptomyces and Bifidobacterium.
Increased Bifidobacterium levels serve as an important indicator of human health and may promote anti-inflammatory activity (Arboleya et al., 2016; Hughes et al., 2017; Tao et al., 2020). It is interesting to note that these same disorders are key risk factors in severe SARS-CoV-2 infection, and Bifidobacterium abundance is also shown to be low in SARS-CoV-2 infection (Tao et al., 2020; Xu et al., 2020; Reinold et al., 2021; Yeoh et al., 2021; Zuo et al., 2021; Hazan et al., 2022b). Probiotics, which typically contain much Bifidobacterium spp., have been proposed as potentially useful SARS-CoV-2 infection prophylaxis or treatment (Bozkurt and Quigley, 2020; Conte and Toraldo, 2020; Bozkurt and Bilen, 2021; Jabczyk et al., 2021).
The mechanisms for Bifidobacterium boosting “natural immunity,” thereby protecting against SARS-CoV-2 infection effects, may involve its anti-inflammatory properties (Lim and Shin, 2020). Specifically, Bifidobacterium increases Treg responses and reduces cell damage by decreasing the function of TNF-α (the pro-inflammatory “master-switch,” see Figure 1A.) and macrophages (Hughes et al., 2017). Bifidobacterium spp. also increase the anti-inflammatory cytokine interleukin (IL)-10, regulate the helper T cell response (Ruiz et al., 2017), and, in a mouse model of inflammatory bowel disease, B. bifidum and B. animalis reduced pro-inflammatory cytokines and restored intestinal barrier integrity (i.e., decreased potential for “leaky gut”) (Ruiz et al., 2017). In short, Bifidobacterium, through TNF-α and interleukins, can decrease inflammation, leading to increased immunity. Moreover, a decrease in pro-inflammatory cytokines and increase in anti-inflammatory ones can help negate the cytokine storm of SARS-CoV-2 infection.
Figure 1
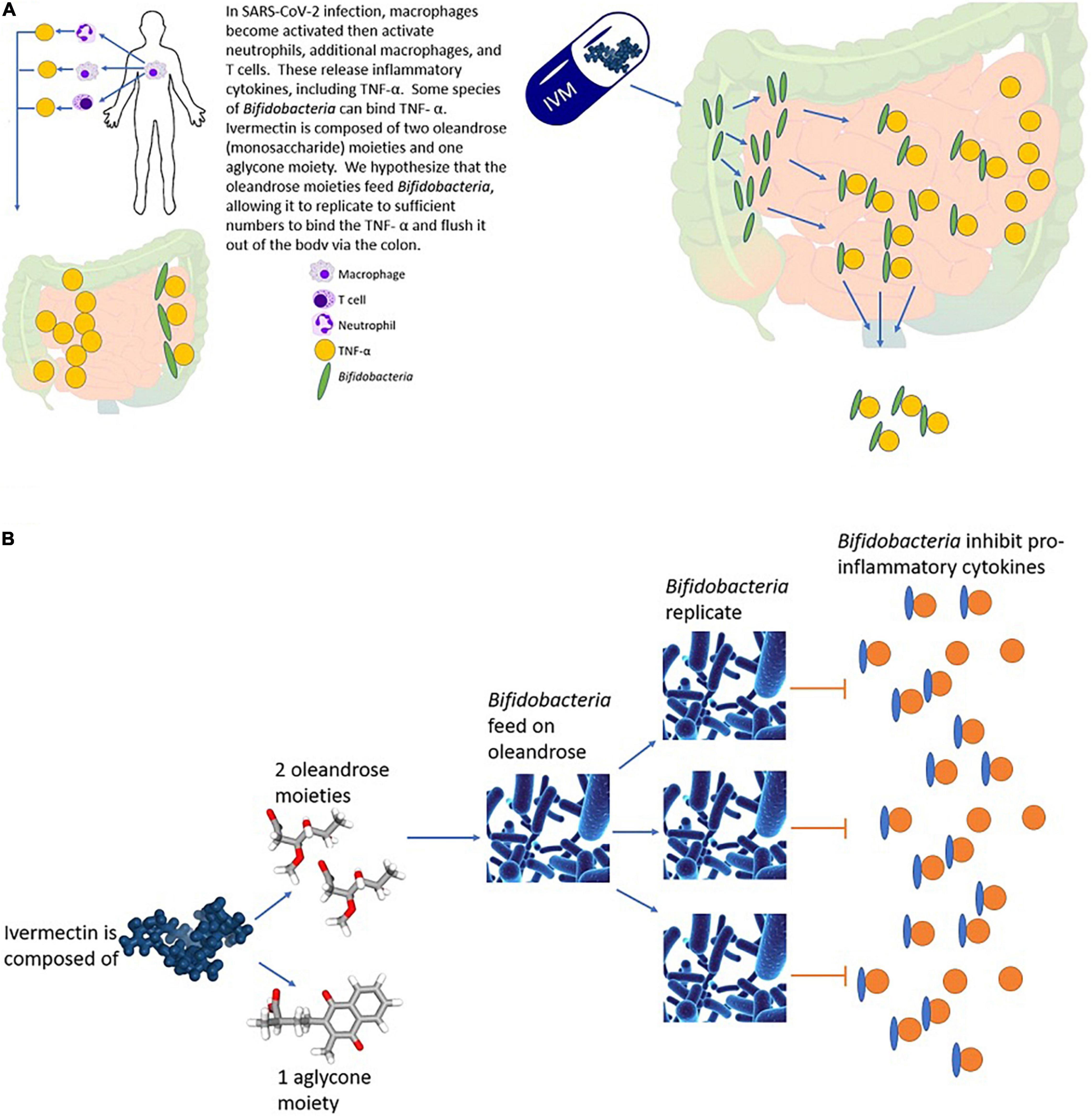
FIGURE 1. We hypothesize that IVM treats SARS-CoV-2 infection by decreasing inflammation through enhanced replication of Bifidobacterium, leading to inhibition of TNF-α. (A) Bifidobacterium inhibits inflammation viabinding of TNF-α. (B) Expansion of the right side of panel (A), showing IVM contains monosaccharide oleandrose moieties that could feed Bifidobacterium, thereby increasing replication and increasing inhibition of TNF-α and inhibition of inflammation.
Hypothesis and Evaluation
Bifidobacterium is a heterotroph that feeds on a variety of carbon sources, but, most efficiently, simple sugars (oligosaccharides and monosaccharides) (Rivière et al., 2016). IVM is composed of two oleandrose (a monosaccharide) moieties, along with one aglycone moiety (Barton et al., 1999; Figure 1B). A naturally found reversible glycosyltransferase, AveBI, can breakdown or assemble IVM to or from these components (Zhang et al., 2006). Thus, IVM breakdown products include oleandrose, a monosaccharide that may feed Bifidobacterium, thereby promoting its growth (Figure 1B).
There may be other mechanisms of action of IVM in SARS-CoV-2 infection treatment. Studies found that IVM has significant potential binding affinity for many proteins within SARS-CoV-2 (Lehrer and Rheinstein, 2020; Saha and Raihan, 2021). Ivermectin could, thus, block the binding of the spike protein’s receptor binding domain within SARS-CoV-2 to the ACE2 receptor (Lehrer and Rheinstein, 2020; Saha and Raihan, 2021). This binding between the spike protein and ACE2 receptor is essential for viral entry. This same study also demonstrated that IVM has the ability to bind a protease on the non-structural protein 3, which serves as a part of the viral replication/transcription complex. This binding prevents the virus using its enzymatic activity to remove ubiquitin, allowing the host anti-viral interferon response to aid viral clearance. Other reviews discuss various proposed mechanisms of IVM in SARS-CoV-2 infection (Heidary and Gharebaghi, 2020; Rizzo, 2020; Kinobe and Owens, 2021).
Discussion
Ours and other data also support a protective role of Bifidobacterium in SARS-CoV-2 infection, possibly through these immune functions of Bifidobacterium. Our study and others (Tao et al., 2020; Xu et al., 2020; Reinold et al., 2021; Yeoh et al., 2021; Zuo et al., 2021; Hazan et al., 2022b) show that the gut microbiome, particularly Bifidobacterium levels, relates to positivity and severity of SARS-CoV-2 infection. Tao et al. (2020) showed that changes in gut microbiota composition might contribute to SARS-CoV-2-induced production of inflammatory cytokines in the intestine, which may lead to the cytokine storm onset.
An increase in Bifidobacterium levels can reduce inflammation levels and TNF-α function, thereby calming the cytokine storm of SARS-CoV-2 infection. Bifidobacterium has been shown to bind TNF-α (Hughes et al., 2017; Dyakov et al., 2020). This binding will absorb TNF-α from the gut, which, in turn, will reduce it in the blood stream, and eventually absorb it from the lungs and other affected areas (the “gut-lung axis”; Cervantes and Hong, 2017; Figure 1).
IVM is known to have antibacterial affects against Staphylococcus aureus and other gram-positive bacteria, which may seem contradictory to its potential to promote growth of another gram-positive bacterium, Bifidobacterium. However, a study by Lazarenko et al. (2012) showed that certain Bifidobacterium spp. can have protective affects against S. aureus infection in mice, thereby acting in an antagonistic relation with S. aureus. Thus, both IVM and Bifidobacterium act against S. auereus, and it is unlikely that IVM would also act against Bifidobacterium.
If this presented hypothesis is true, the timing of IVM administration should be just prior to or at the cytokine storm. Seriously affected SARS-CoV-2-infected patients develop a cytokine storm alongside hypoxemia around Days 10–14, referred to as the “Second week crash” (Bernstein and Cha, 2020; Mehta and Fajgenbaum, 2021; “Second-week crash” is time of peril for some patients with COVID-19). Our study on IVM combination therapy initiated therapy around Day 10, as patients typically presented to the study hypoxic at Day 9 (mean time from the symptom onset to treatment initiation was 9.2 days). This timing resulted in successful treatment, with all 24 severely hypoxic patients, recovering without hospitalizations (Hazan et al., 2022a). In short, IVM should typically be administered at the point of an SpO2 drop, the cytokine storm onset, and/or approximately Days 10–14.
Conclusion
We are hypothesizing the IVM mechanism of action as a therapeutic for COVID-19 is through feeding of Bifidobacterium, which then inhibits cytokine function and tames the cytokine storm (Figure 1). As such, IVM should be administered at the time of the cytokine storm.
