Harvard says so, therefore it must be true. And Circulation printed it. But it took 6 months to get through review.
https://www.ahajournals.org/doi/epdf/10.1161/CIRCULATIONAHA.122.061025
Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis
16 young people aged 12-21 who were hospitalized with myocarditis soon after a COVID shot were compared with 45 controls in the same age group. Two findings stuck out to me. First, there was no evidence of autoimmunity (antibodies against self-antigens) in the subjects.
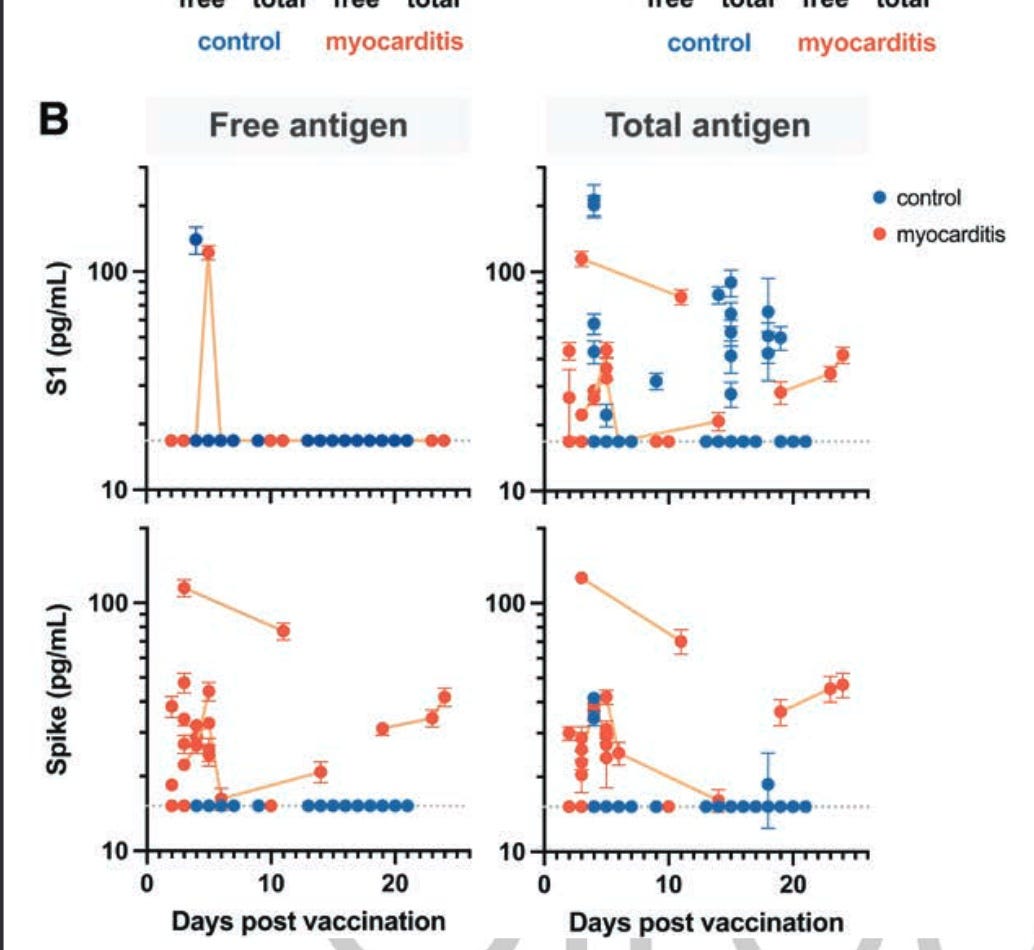
Second, full length spike protein was found in the plasma of most of the myocarditis patients but in almost none of the controls. Cleaved spike subunit (S1) was not found differentially, but the full length product of mRNA vaccine translation was found. Most was free, unbound to antibody, which I found surprising. The difference between the myocarditis cases and controls is impressive.
Are the kids who develop myocarditis simply those whose vaccine ‘worked better’ and led to considerably more spike protein production? Could the answer be this simple? Or was their ability to bind spike overwhelmed?
The authors wrote,
both free and antibody-bound spike, which was detectable only in patients who developed vaccine-induced myocarditis, remained detectable up to 3 weeks after vaccination.
They also stated,
There is growing in vitro evidence that spike itself can stimulate cardiac pericytes dysfunc-tion23 or inflame the endothelium, potentially by down-regulating angiotensin-converting enzyme 2 expression, by impairing endothelial nitric oxide bioavailability,24 or by activating integrin-mediated inflammation with hyperper-meability of the endothelial cell layer.25 Thus, the spike antigen itself, which evades antibody recognition rather than invoking immune hyperactivation, may contribute to myocarditis in these individuals.
And in the end, of course the authors took a knee:
Although the implications of this finding must be better understood, these results do not alter the risk-benefit ratio favoring vaccination against COVID-19 to prevent severe clinical outcomes.
What I found interesting was that it took 6 months from submission to acceptance, despite this being a landmark study of great public health interest.
Source – https://merylnass.substack.com/p/adolescents-and-young-adults-with