
Covid vaccination increases the risk of severe heart inflammation up to 120-fold, a major study from Scandinavia published in the Journal of the American Medical Association (JAMA) has found.
The study looked at over 23 million patient records covering the over-12s populations of Denmark, Finland, Norway and Sweden from the start of the vaccine rollout in December 2020 to October 5th 2021.
For young males aged 16-24 years within 28 days of a second dose the study found severe myocarditis (requiring inpatient hospital admission) around five times more common after Pfizer and 14 times more common after Moderna. This corresponded to six events per 100,000 people after Pfizer and 18 events per 100,000 after Moderna. A second dose of Moderna given after a first dose of Pfizer came with even higher risk: a 36-fold increased risk, corresponding to 27 events per 100,000 people. The Moderna vaccine has three times the dose of mRNA of the Pfizer vaccine, which the authors suggest lies behind the increased risk.
The authors observe that of the 213 severe myocarditis cases in the 28-day risk window after a second dose of mRNA vaccine, 135 occurred within the first week. This is more than half, meaning the risk in that week is greatly elevated. Among males aged 16 to 24 years, the risk was around 13-fold greater during the week after a second dose of Pfizer and 38-fold greater after a second dose of Moderna. For a second dose of Moderna where the first dose was Pfizer the risk was 120-fold greater.
It’s worth noting that the bar for myocarditis here is very high, excluding even those who receive medical attention as a hospital outpatient, let alone anything milder; even the milder cases, however, may cause long-term damage.
The study found that the severe myocarditis risk following Covid infection was negligible, with only around one excess event per 100,000 within 28 days of infection and a confidence interval that included zero.
For some reason the study did not look at the risk outside the 28-day post-vaccination window, so we don’t know whether the elevated risk continues past that period.
It’s worth bearing in mind that the risk estimates are adjusted estimates based on modelling that takes into account potential confounding factors: sex, age group, health care worker status, nursing home resident and certain listed comorbidities. The unadjusted risk estimates are not stated, and we do not know how sound the adjustments are. It’s not clear why it was necessary to use modelling to adjust for these factors rather than, say, simply providing results stratified by sex and age and with health care workers, nursing home residents and people with comorbidities excluded, at least from some of the results. Modelled adjustments are often opaque, especially when unadjusted estimates aren’t provided, whereas stratified findings are usually clear.
The results were summarised as follows:
Among 23,122,522 Nordic residents (81% vaccinated by study end; 50.2% female), 1,077 incident myocarditis events and 1,149 incident pericarditis events were identified. Within the 28-day period, for males and females 12 years or older combined who received a homologous schedule [two vaccine doses of the same type], the second dose was associated with higher risk of myocarditis, with adjusted IRRs [incidence rate ratios] of 1.75 (95% CI [confidence interval], 1.43-2.14) for BNT162b2 [Pfizer] and 6.57 (95% CI, 4.64-9.28) for mRNA-1273 [Moderna]. Among males 16 to 24 years of age, adjusted IRRs were 5.31 (95% CI, 3.68-7.68) for a second dose of BNT162b2 and 13.83 (95% CI, 8.08-23.68) for a second dose of mRNA-1273, and numbers of excess events were 5.55 (95% CI, 3.70-7.39) events per 100,000 vaccinees after the second dose of BNT162b2 and 18.39 (9.05-27.72) events per 100,000 vaccinees after the second dose of mRNA-1273. Estimates for pericarditis were similar.
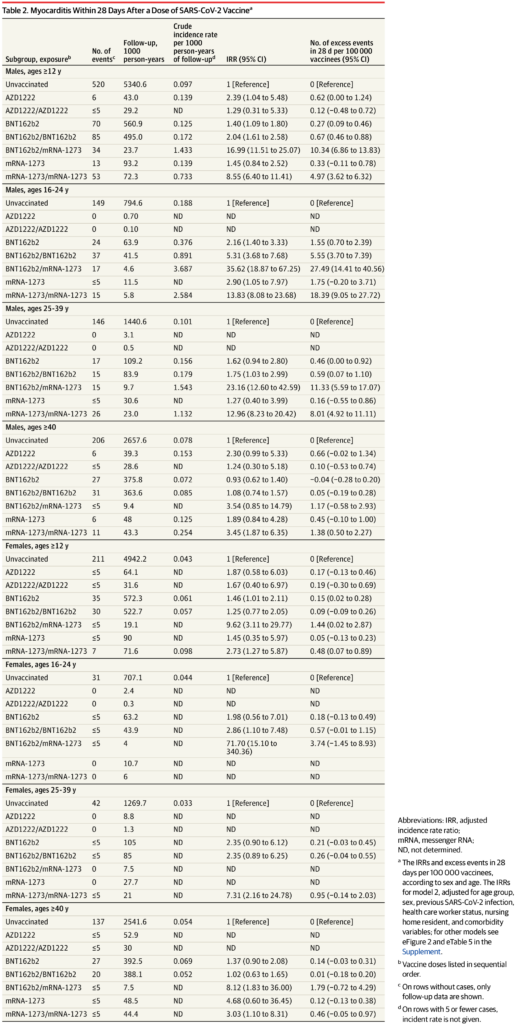
Here’s the complete table of results for severe myocarditis in the 28-day window. Note that the risk is considerably elevated for many subgroups, particularly for males under 40 (not just aged 16-24) following a second Moderna dose, but also in other cases too. However, the wide confidence intervals make the findings uncertain in many subgroups outside males under 40.
The authors conclude the risks “should be balanced against the benefits of protecting against severe COVID-19 disease”. However, given the extremely low risk of Covid to healthy young males and the considerably elevated risk of severe myocarditis following vaccination – plus the risks associated with other adverse effects, short and long term – it’s hard to see how it could be worth it, or why these vaccines have not already been withdrawn for younger age groups.
