
There follows a guest post by Ramesh Thakur, Emeritus Professor at the Australian National University and former Assistant Secretary-General of the United Nations, who is based in Ocean Shores, NSW, Australia.
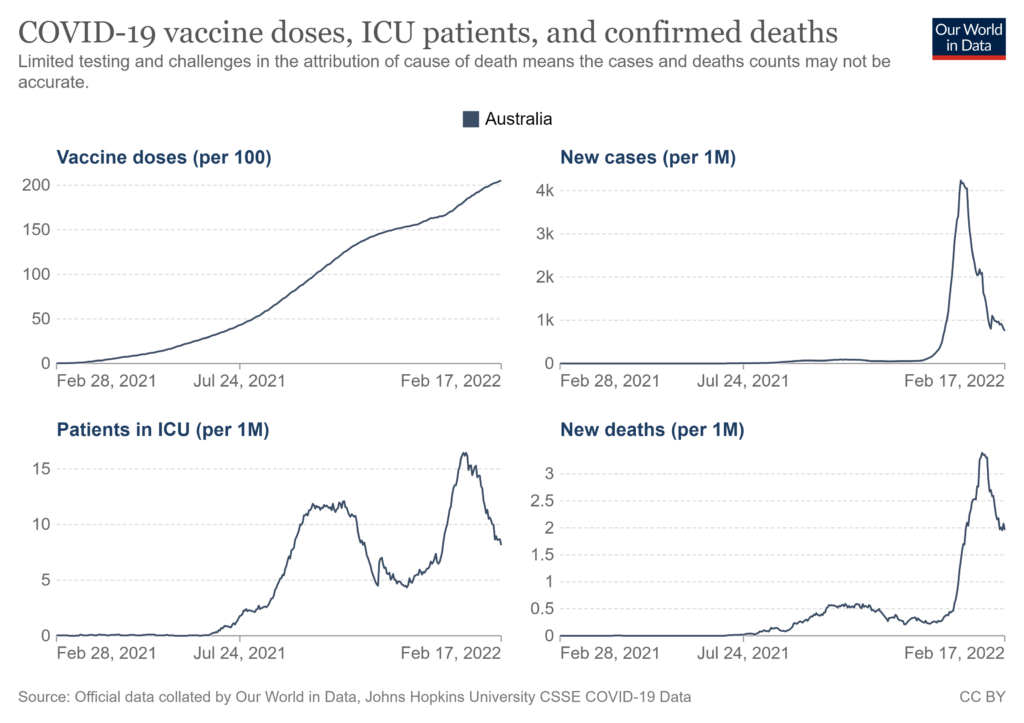
What does the Australian experience teach us about the efficacy of Covid vaccines? Why, for instance, have infections and ICU admissions been hugely higher after vaccination campaigns really got under way? Australia hit 50% of the population double-vaccinated (meaning a much higher percentage of the adult population) on October 10th 2021, and 70% in mid-November. On October 10th our total Covid-related deaths were 1,448. On February 15th 2022, with 79% of the total population fully vaccinated, the total number of deaths was 4,726. So the number who died with Covid after we hit 50% vaccination is 2.3 times higher than the number before that point.
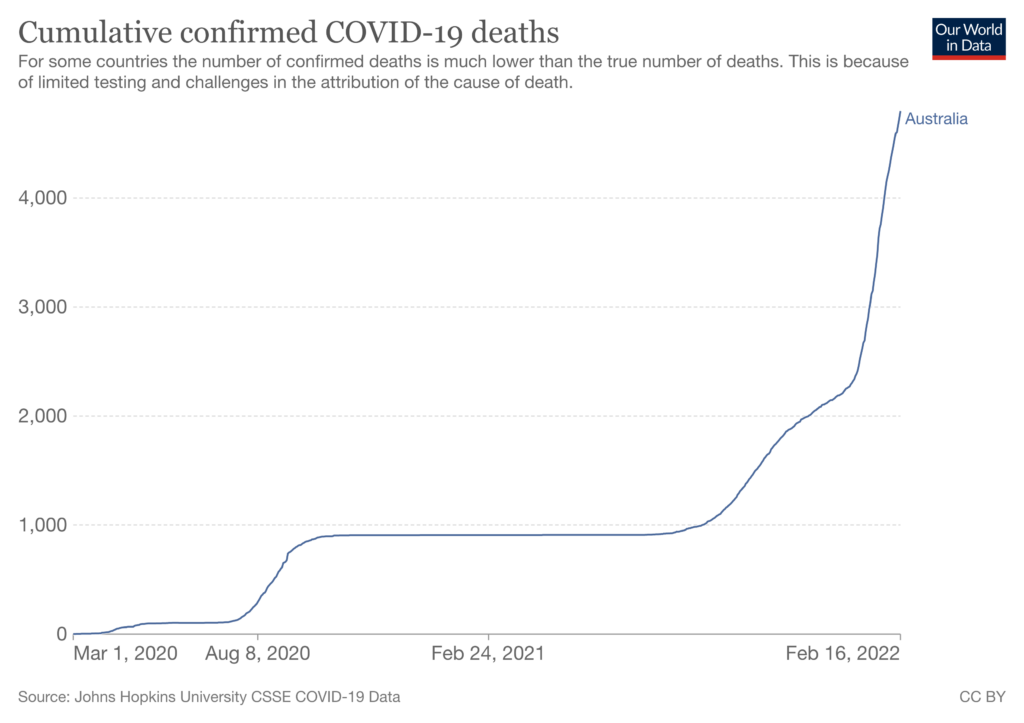
To come to the same conclusion from a slightly different angle – Our previous highest Covid mortality rate was 0.85 daily new deaths per million people, on September 3rd 2020. On that date, vaccines had not yet been developed anywhere in the world. The rate was exceeded on January 11th this year with 0.97 daily new deaths per million people, when we had 77.5% of the total population fully vaccinated. The rate peaked on January 30th at 3.39 daily new deaths per million people: four times higher than the pre-vaccination peak. At this time 78.3% of the population was fully vaccinated.
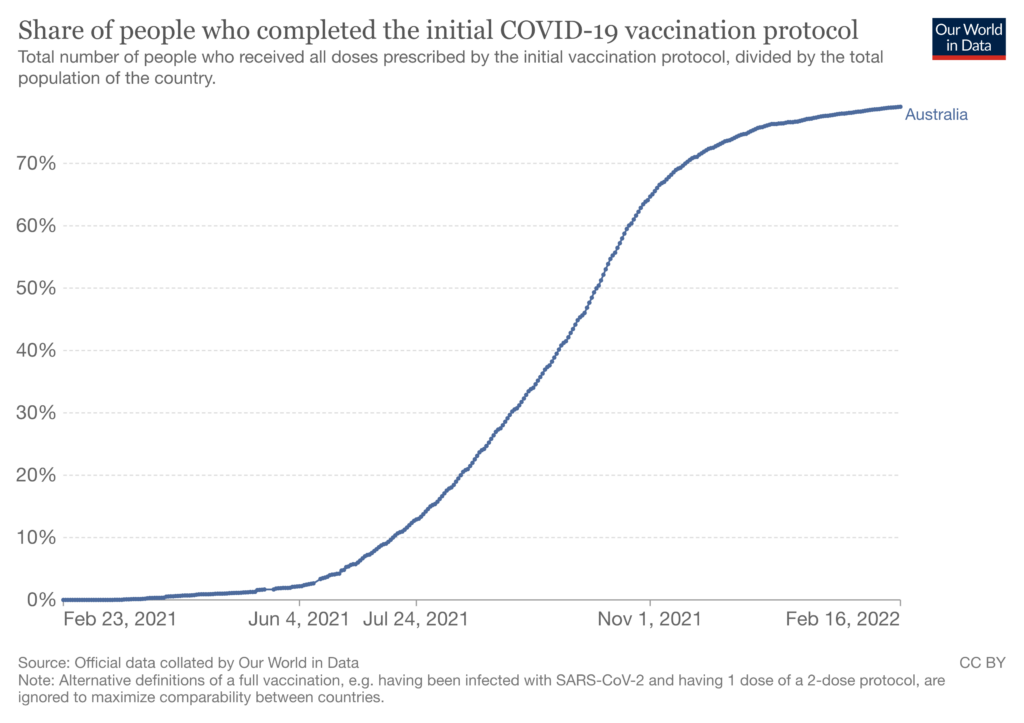
Now let’s look at ICU numbers, especially as this has been the most often cited public justification for encouraging and requiring vaccination. The pre-vaccines peak was on August 9th 2020 with 2.17 ICU patients per million people. The highest rate of ICU daily occupancy was on January 18th this year, 16.44 ICU patients per million people.
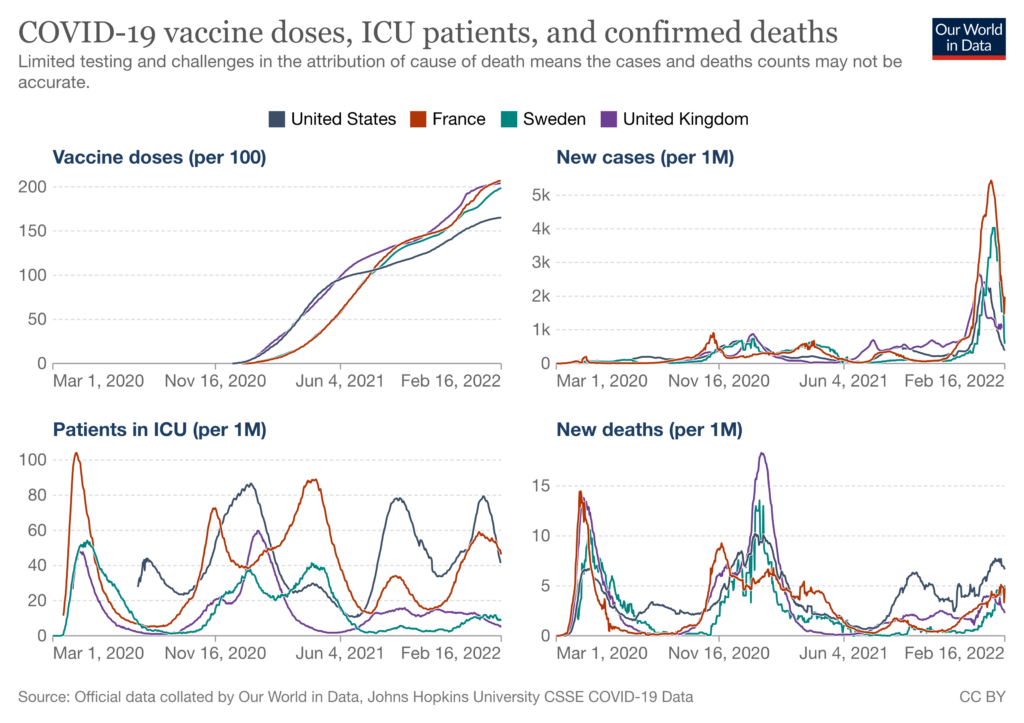
Finally, we see a similar absence of correlation between vaccination and COVID-19 infection, ICU and mortality rates in four major country examples: France, Sweden, U.K. and USA.
I am not questioning the decision of any individual to get vaccinated. I am double vaccinated.
Rather, what I am asking is: How can it possibly be justified to mandate universal vaccination on this data? This is simply not defensible on medical and ethical grounds. Globally and in Australia, hard data clearly show there is no discernible difference in transmissibility between vaccinated and unvaccinated of any significance to base policy on.
Finally, does the country, or any private company or public entity including a university, really want to lock itself into a never-ending cycle of boosters, which is a very real prospect both on overseas trends and also on the numbers of vaccine doses Australia has already purchased or ordered?
What the data do show is continuing strong protective benefits of the vaccine for the elderly and vulnerable. What might make more sense would be to make the vaccine compulsory for people 65 and older – not that I am suggesting that older people should be compelled in this way to have regard for their own safety, as they may wish to assess the equation differently, which they should be entitled to do. But such a policy – though still illiberal and unethical – would at least have some kind of evidence behind it, which universally mandating this vaccine plainly does not.
